As part of the BSc Radiotherapy and Oncology course at Sheffield Hallam University, the final 2 weeks of second year in September (yes, students still haven’t technically finished second year even in September!!) are used as a self-funded, optional elective placement.
When thinking about where to go for elective, a million (okay, maybe just 20 or so) different locations came into my head… Canada? The USA? Europe? However, I had to think logically and realistically and as exciting as those places may have been, I knew I needed to start giving some serious consideration as to where I would (eventually and hopefully) want to work.
As my bio highlights, I am born and raised in Essex, or “down South” as my course-mates name it, therefore used my hometown as a base location. Eventually, after writing and re-writing request letters, the two departments I was fortunate to receive placements in were University College London Hospital (UCLH);

and Southend University Hospital;

University College London Hospital:
Bright and early on Monday morning, I had to forget the friendliness of t’up North that I had grown used to and put on my dusty London commuter hat again. After my 50 minute or so journey of standing and avoiding contact with anyone, I made it to UCLH. I automatically made my way to the basement as, let’s face it, that’s where all radiotherapy departments are. I was greeted by one of the superintendent radiographers and given a tour of the department. My initial thought was how quiet the department was in comparison to the very large department I was accustomed to up North!
My first day was spent in pre-treatment (which includes CT-Sim, VSim and mould room). Some things I found very interesting were the method in which the department immobilises limbs for treatment. A polystyrene block is used as an indexed base, with a styro-foam type material which is sprayed and the patient’s limb put onto so that it moulds around them conformally. Once this has set, pieces of thermoplastic are heated in a water bath until pliable and these pieces are then moulded over places such as the knee, elbow, thigh etc. and clipped onto the base. The patient is then also tattooed in 2 or 3 places and, if it is the leg that is being treated, the contra lateral limb is lifted onto a Perspex bridge, allowing for lateral beams to be used. I think that this immobilisation technique is really efficient as it is not only comfortable for the patient, but it is more accurate (due to the indexing) and much more reproducible (due to the thermoplastic holding the limb in the same place each time and simplicity of set-up). Limbs are renowned to be difficult to scan in pre-treatment in terms of set-up technique, however, immobilisation methods such as this is an example of how departments can learn from each other using evidence based practice. Another, more fun, difference was the fact that paediatric patients who need to have a mask made can choose from a variety of temporary tattoos (anything from Hello Kitty to Iron Man!) with which, the mould room staff will decorate the mask ready for treatment, helping paediatrics to comply with treatment a lot better and making it a more patient focused service.
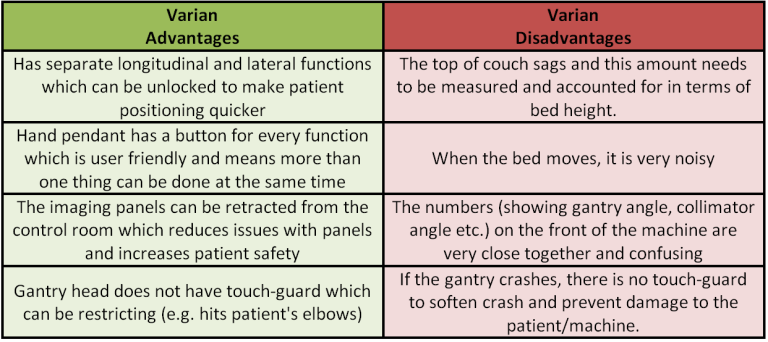
Over the next few days I was to be placed on the linear accelerators themselves and get more involved in the actual treating of patients! Now, coming from an Elekta department, I realised I would have to ‘fraternise with the enemy’ and use Varian machines for the rest of the week! I have written a few of my top praises and criticisms of each brand of machine;
So overall, there is no clear winner in terms of which I prefer!
As well as differences in machines, there were vast differences in practice, from the actual techniques themselves to how the diary is managed;
- Firstly, it felt really good to not have to lift a breast-board (that is about half the height of me!) all the way from one side of the room to the treatment couch on my own. Instead, UCLH are really on top of their moving and handling, making sure that all staff push heavy items of immobilisation equipment on a trolley and that the bed is raised to working height when cleaning it etc. which saved my back a lot of hassle!
- There was one major change that I struggled to get used to – using maths again! At my placement department I have gotten used to using the Couch Move Assist function which moves the couch from the reference marks to the isocentre (treatment position) in all directions automatically. However, at UCLH (and Southend) this is worked out manually by the radiographers therefore my quick mental maths skills had to be dug up from the ‘A-Level maths’ part of my brain!
- Earlier I mentioned the fact that for Varian machines you have to work out the ‘sag’ on the bed. This is done by taking the couch up to where the coronal laser is in line with the top of the couch. The value of the couch height at this point is taken away from 1000 (e.g. 1000 – 999.7 = 0.3). This value is then the SAG, this is noted down and taken away from the isocentric couch height. Make sense? Good, because there’s more! For each machine (as the patients changed linacs a few times) a SAG calculation has to be made on 3 separate occasions before a mean SAG can be calculated and used for every treatment on that linac thereafter. Sometimes I questioned how accurate this calculation was and how much of a difference this made to the treatment itself.
- Another difference in practice was the fact that the department didn’t seem to check SSDs that much! However, I suppose this is made up by the fact that kV imaging is done daily and CBCT imaging done weekly on a majority of patients. I guess that a reason my placement department do not image on every fraction is because of the high capacity to which the department treats (around 35-40 patients on each machine a day with 9 machines in clinical use daily means roughly 315-360 patients treated a day, compared to the 85 or so patients that are treated at UCL in a day) and of course imaging frequently means a larger appointment slot. However, at my clinical placement department, someone having an image, which is then reviewed online, gets the same length appointment slot that a patient not having an image gets, meaning it is easy to get behind, particularly if there is something wrong with an image, however, at UCL, there is daily imaging so it’s okay that appointment slots are the same length.
- One thing I knew would differ between departments was the protocols regarding bladder filling and rectal status for prostate patients. Something I found interesting at UCL was the fact they ask their patients to come into the department around one week before their planning CT scan to go through the procedure with them. They then ask the patient to start using the enema daily from that appointment onwards and to start drinking more water each day to sort of ‘train’ their bladder. The department have found that this helps with patient compliance and it means that the patient is aware of the procedure by the time the CT planning scan and treatment commences. This is something my placement department could perhaps trial as I have noticed that patients struggle with the protocol around a week into treatment as their bladder isn’t full enough or they can’t hold as much because they have been told to drink more water generally. However, this would obviously take more time and mean an extra hospital trip for the patient.
During my time at UCL, I had requested to spend some time with the paediatric team as I knew the department treated a lot of children from Great Ormond Street Hospital. I was fortunate enough to spend some time with the play specialist and visit the paediatric and teen/young adult play rooms. My placement department have literally just opened a teen ‘chill out’ area (which I haven’t seen yet!) so it was good to see one in use. I was also fortunate enough to spend some time in a clinic with one of the paediatric oncologists and learnt a lot about paediatric tumours (one of which I had more knowledge of than the 4th year medical student who was in the room with me!) and the consent process. I followed through one patient who was having Total Body Irradiation (TBI) before his bone marrow transplant into clinic where is consultant explained what radiotherapy was and why he needed it. This was before the play specialist took the patient on a tour of the department and showed him a video which described the whole TBI procedure (including the CT scan), what he needed to and what the role of the radiographers are. It was really interesting to see how the consent and information supplying procedure in terms of method and language and resources used differed from adult treatments.
In summary, my first impression of the department was how quiet it was, as I mentioned above, I am used to nearly 400 patients (plus relatives/friends/carers too!) being in the department in one day. However, I found the staff to be really lovely to work with and they all seem to get on really well with each other. Lots of the staff were doing or have done a masters in the radiotherapy field, showing continual professional development and they seemed really encouraging when it came to discussing my dissertation topic. Overall, I found it a pleasure to spend a week there, learnt an awful lot and is definitely on my list of departments I would like to apply for should any band 5 jobs become available.
Southend University Hospital:
I decided that it would be cheaper for me overall to drive to Southend hospital and pay for parking than to get the train from Upminster to Southend and get a bus or cab. This made the commute a lot less crammed than my tube experience the previous week! The commute overall took me about 30 minutes, however, I thought that there would be way more traffic than there actually was and ended up getting there at 7:35am on my first day, a whole 55 minutes early (definitely something I corrected for the rest of the week!). I had to make my way to the Radiotherapy reception and definitely thought I had missed it completely because the department is quite spread out through a series of twists, turns, doors and corridors but eventually I found it! I was greeted by one of the Advanced Practitioner Radiographers took me on a tour of the department and gave me a timetable of my week.
Immediately I felt more at home as the department used Elekta machines (hallelujah!) however, they still didn’t use the Couch Move Assist function (boo!) so the rusty maths skills had to be dug up again. For the rest of my first day I was placed on one of the Linacs and I was fortunate enough to be placed with a new starter/recent graduate. Observing her and talking to her helped me to understand the whole preceptorship process a lot better. She was a City University graduate who had undertaken her training at the Addenbrooke’s Hospital in Cambridge, therefore Southend hospital was new territory for her and it was great to see how happy she was there and how she had already fitted into the team after only being there for a month.
I was also able to spend some time in the VSim department where one of the radiographers talked me through breast planning and how it is becoming more radiographer than clinician lead. The breast technique is very complicated at Southend (I’ll explain further later!) so it was really useful to be talked through how they plan the beams and reach the measurements that are involved in the set-up as it helped me understand the technique as a whole. That day I was also able to shadow one of the specialist radiographers undertake a clinic for prostate patients. These clinics were attended by the patient on a weekly basis and it gives the radiographer an opportunity to asses the patient’s quality of life in terms of how they are coping with treatment and the side effects they are experiencing as well as offering advice and information on the future (e.g. life after radiotherapy has finished? what Brachytherapy involved? etc.). I think clinics like these are extremely beneficial to the patient as it allows them to connect to the radiographers and for any issues to be ironed out along the treatment pathway. Furthermore, because the clinic is run by a radiographer, they understand the radiotherapy process, the treatment itself and the side-effects a lot better than maybe a doctor would as they are on the ‘front line’ and understand the techniques and the theory behind them.
Once again, there were quite a few differences in practice which are outlined below;
- Firstly, that crazy different breast technique I was talking about?! Essentially the patient is lying on a breast-board with the arm of the breast that is being treated raised and resting in some cups. First of the all the borders of the field are drawn on (measurements from tattoos are on the set-up sheet). Then (from what I can remember) the bed is moved so that the cross hair is in line with the anterior tattoo and the height is raised so that the laser is on the lateral tattoo. Then the gantry is rotated to an angle where the back-pointer laser is in line with the lateral tattoo. Then these bed values, the gantry angle and some measurements that are fixed on the set-up sheet are put into this Excel spread-sheet which works out the bed height and lateral position at the isocentre as well as what the gantry angles should be for the medial and lateral field. These angles are then checked using the field light and the borders drawn on in the first step. Once the field light matches these borders, the gantry angle is checked to make sure that it is within 2 degrees of the angle worked out by the excel spread sheet. This is also checked when doing the second field. Make sense?
- Like UCLH, CBCT imaging is daily.
- Prostate patients are required to have a full bladder for treatment, which is pretty standard practice. However, Southend Hospital use Milk of Magnesia as a liquid laxative instead of micro-enemas. Initially the patient is to take 25ml of this a day, the reasoning behing this is that radiographers are allowed to prescribe up to 50ml a day so they have decided to start in the middle so that they have flexibility either way to either reduce or increase the dose. The dose is also reviewed in the weekly prostate clinic depending on how it is effecting the patient’s bowels and quality of life.
- Breast and chest patients get a special gown to wear for treatment. The gown had poppers in the middle and along the shoulders (see image below). This meant that patients only needed to get the side out that was being treated and was a lot easier for patients to wear (compared with putting on a generic hospital gown back to front and worry about it falling down or being bunched up etc.)

(REF: http://www.hey.nhs.uk/news/hospital-staff-make-things-better-by-design.htm)
Overall, I really enjoyed my time in this department and once again I found everyone to be so friendly and welcoming! The elective experience has taught me an awful lot in all aspects of Radiotherapy, whether it is in patient care, treatment techniques or the logistics and running of a department. I am really grateful for my time at both of these departments and for all the staff that took me under their wing for the time that I was there. It has broadened my skills and knowledge, made me realise that I know more than I thought I did, improved my confidence and helped me to meet some lovely people.
I would definitely consider applying to both of these departments for jobs, so I’d best get on with completing my final year of undergraduate study and register with NHS jobs!
Charlotte